“Listen to your patient. Only then have you a chance to come up with truly the best solution for his or her eyes.”
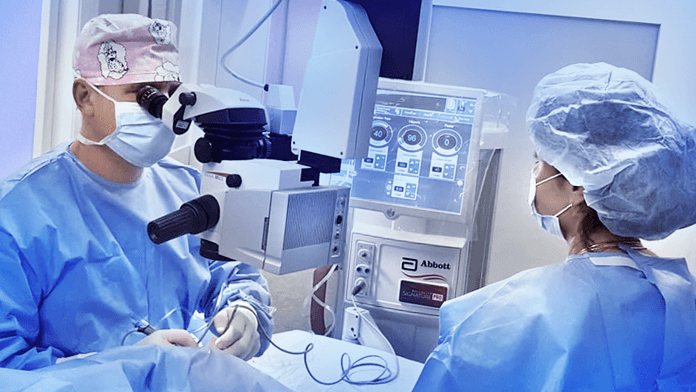
Top specialists
Your eyes will be in the hands of top specialists in the field of diagnostics and eye surgery. Our clinic is state of the art and we are one of the most experienced teams in the Czech Republic.
Patient care
We take pride in getting to know our patients as the individuals they are. Being a small-scale clinic, we offer a tranquil and friendly environment and are available to be of help 24/7.
Opening Hours
Monday8.00 – 17.00
Tuesday8.00 – 20.00
Wednesday8.00 – 17.00
Thursday8.00 – 17.00
Friday8.00 – 16.00
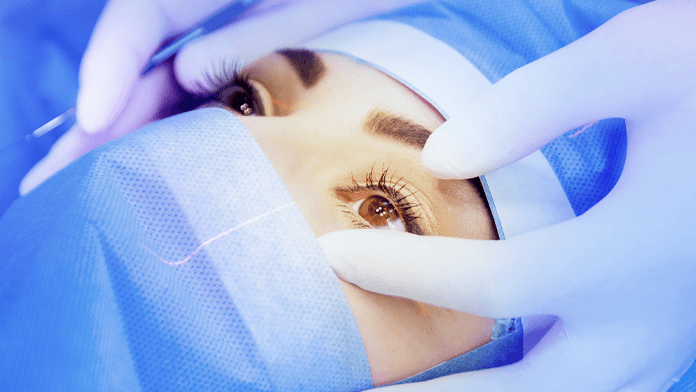
Professional Approach
We carry out in-depth examination of your eyes based on which we recommend a tailor-made solution just for you, be it lenses, glasses or surgical procedure.
Remarkable Experience
We have been on the ophthalmological market for over twenty years bringing excellent results to our Czech as well as foreign patients.
Mutual Trust
We maintain long-lasting personal relations with our patients. We know their problems and bestow on each as much time and attention as is needed.
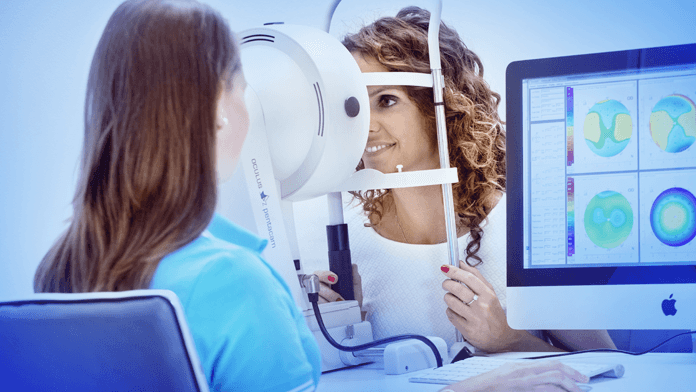
Latest Technology
We care for your eyes with the help of modern, state of the art medical technology and equipment. We are proud to work with only premium diagnostic machines.
For your eyes
What they have to say about us
Meet the experts

Dr Petr Novák
Eye surgeon, specialist in cataract, corneal and refractive surgery

Dr Sylva Procházková, PhD.
Eye surgeon, specialist in cataract and refractive surgery
“A satisfied patient is the very best review of our team’s work.”

Dr David Klečka
Eye doctor, specialist in refractive surgery
“I only ever recommend to my patients a solution that appears most suitable and smart in the given case.”
We are qualified
Certificates
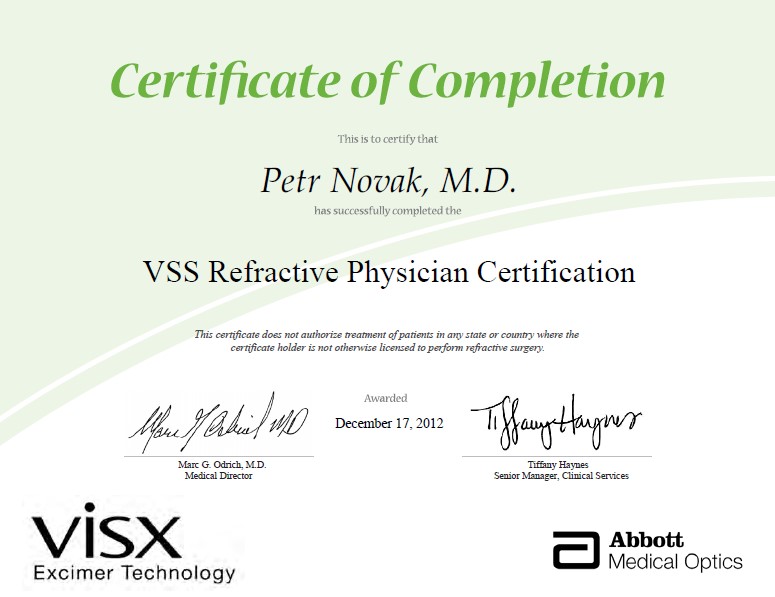

We keep on acquiring the latest findings so that we are on top of our game where the newest ophthalmological trends are concerned.